
Dorothy Masasa dey happy dey waka for di dirt road one sunny afternoon, she carry her pikin for back.
Six months ago, di 39 years old woman wey from Thyolo district for southern Malawi go Kenya to do radiotherapy to save her life.
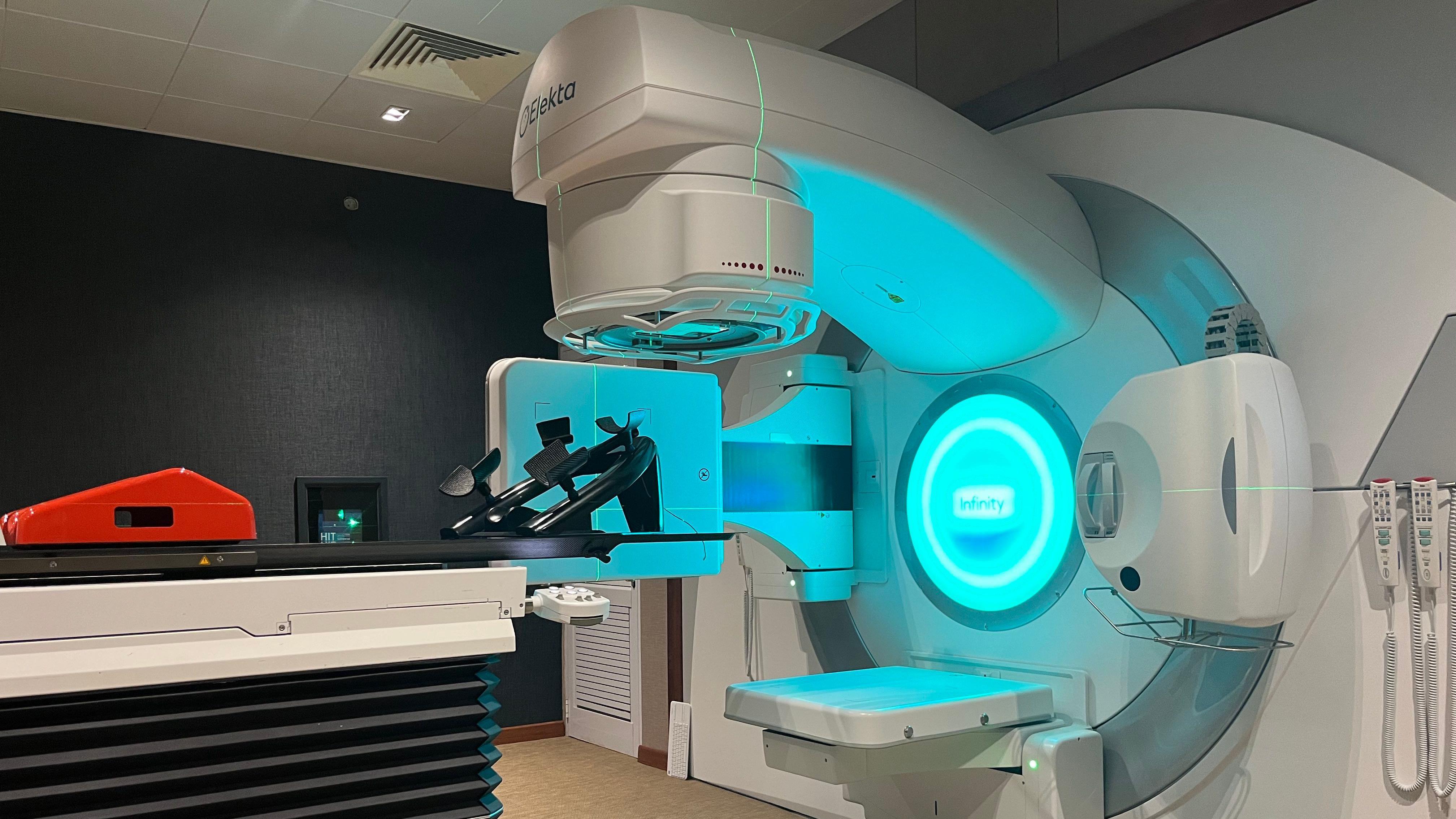
Malawi only recently finally get dia own machine, so odas way wan do radiotherapy no go need to travel abroad for di treatment.
“Dem register me as emergency case after doctors find out say I get cervical cancer wen I still dey 13 weeks pregnant. Dem tell me say di two no fit go together “na wetin di mother of three tell BBC.
She say di doctors for Malawi tell am say she fit do surgery to remove di cancer but e fit terminate di pregnancy, or she fit do chemotherapy but e go put di life of di baby inside at risk and e fit cause am disability wen dem born am.
She decide to do di chemotherapy until dem born di baby through caesarean section – without any disability.
Dem remove her uterus during the surgery.
Before dem diagnose am, she bin dey get cramps for her lower abdomen, plus bleeding and vaginal discharge wey dey smell and no wan stop. Di doctors been dey think say na sexually transmitted infection.
Even after di chemotherapy and surgery, she still need further treatment to cure di cancer, dis treatment bin no dey for Malawi until early dis year.
She join one group of 30 women wey dem carry go Nairobi Hospital for Kenya, Na aid agency Médecins Sans Frontières (MSF) carry dem go di trip to do radiotherapy wey go kill di cancer cells.
Dis na di first time she go travel inside aeroplane, so she dey worried and bin no wan leave her small pikin travel.
“But unto say I dey go collect treatment, I encourage myself to go get di treatment, and I go come back home healthy and happy.”
Wen BBC visit am for hospital, Ms Masasa still dey weak from di effect of di treatment, as she don loose weight and her hair.
She be one of di 77 patients wey dem use plane carry from Malawi to Kenya for cervical cancer treatment since 2022.
Sixty years after dem get independence from di UK, na for March dis year Malawi just install dia first radiotherapy machine for International Blantyre Cancer Centre wey private pesin get, dis na big step for di kontri healthcare system.
More Machines land for June and dem go place am for di National Cancer Centre wey dem still dey construct for dia capital Lilongwe.
Although Malawi still get a long way to go to provide comprehensive cancer treatment, dem still better pass plenty Oda kontris for di region.
For Sub-Saharan Africa, more dan 20 kontris no get access to radiotherapy wey be major procedure dem dey use fight cancer.
Dis mean say patients go travel on expensive and tiring trips to get treatment.
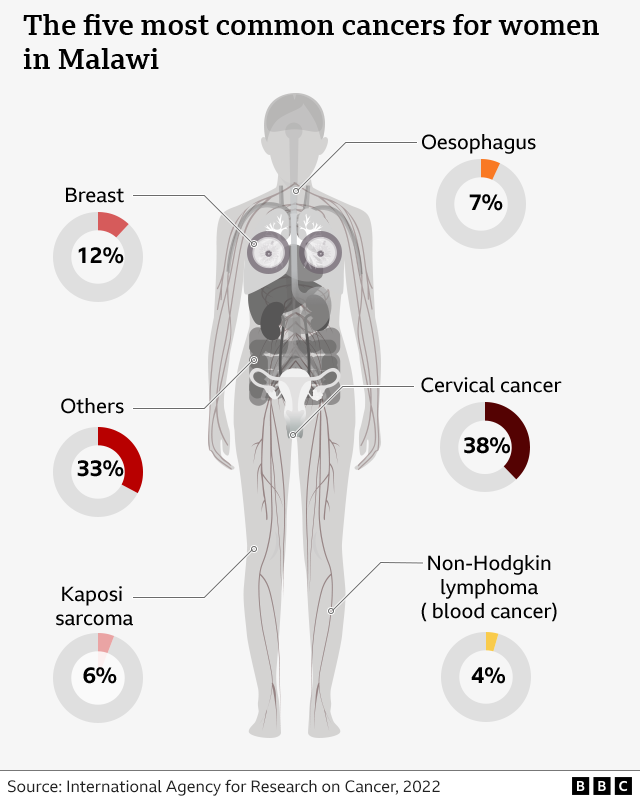
Cancer of di cervix be di fourth most common cancer among women worldwide, e get estimated 660,000 new cases and 350,000 deaths wey dem report for 2022, according to World Health Organisation (WHO).
WHO say 19 out of di 20 kontris wey dey list of kontris wit di highest rates of cervical for 2018 dey for Africa.
Queen Elizabeth Central Central Hospital (QECH) na Malawi oldest goment owned treatment centre. E dey receive a huge number of cervical cancer patients from across di kontri.
Obstetrician and gynaecologist for di hospital, Dr Samuel Meja, say cervical cancer na big problem for most kontris for di region.
“Poor access to screening and di HIV palava wey bin don dey sama parts of di sub-Saharan Africa don dey worst”, na so e tok.
For 2018, Malawi turn out to be di second to only Eswatini for Southern Africa kontris wey get di highest rate of cervical cancer for di world.
Outgoing WHO regional director for Africa, Dr Matshidiso Moeti, say globally, one woman dey die of cervical cancer every two minutes. Africa dey account for 23% of di deaths.
To reverse di statistics, Africa don do ogbonge campaigns to vaccinate girls against di HPV wey dey cause cervical cancer.
Lesotho don reach 93% coverage after dem vaccinate 139,000 girls against HPV.
But stigma around cervical cancer for various African kontris don affect di numbers of pipo wey dey go for vaccination.
In Zambia, for instance, dem dey frown at any pesin wey wan to talk about anything wey relate to gynaecology.
For Malawi, Dr Meja say dem don introduce cervical cancer screening.
“Dis na very simple strategy dem dey use identify women wey dey at risk and treat dem before dem go become cancer patients. Dis investment na wetin we need to make as a nation before matter go comot for hand,” na so im tok.
As for Masasa, she don come back home to Malawi.
Di treatment she collect for Kenya don give am a new lease of life. Her hair don grow back, she fit walk around with her baby for her back, take care of her cow and work for di fields.
She tok say she now know say dem fit treat cervical cancer and say di vaccine fit help oda women avoid di disease, she no get doubt to vaccinate her daughter.
“Cervical cancer take me through hard phase and I no go want make my daughter go through di same wahala,” na so she tok.
“Plenty difference dey between how I dey now and how I bin dey before. I dey so happy say I don dey healed.”











